Dear Dr. Abbasi-Hoskins:
Thanks for your response regarding my 25th rejection to become a member of ACOG’s Medically Underserved Women’s Committee. Please be advised that I will not be submitting any future applications.
Although I have paid my annual dues for the past 25 years, I cannot guarantee that I will continue to do so in the future.
Have you noticed the dwindling number of obstetricians-gynecologists who pay their dues, especially those who look like me?
Although I originally planned to write a lengthy letter, my former high school photographer teacher (may he rest in peace) once said, “A picture is worth 1,000 words.â€
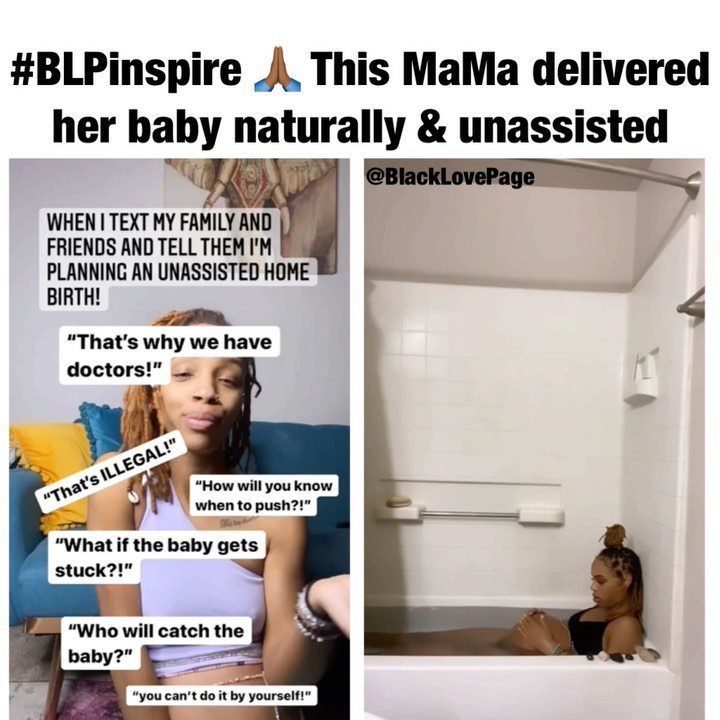
The picture of this Black woman’s unassisted homebirth speaks volumes and represents our dismal failure as effective clinicians in keeping pregnant women safe and unharmed. Some Black women would rather stay home and deliver their babies in a tub without assistance than come into a hospital where they are often disrespected, ignored, and clinically mismanaged. How do we change that narrative?
This week’s JAMA opinion hits home. Medicine is an art as well as a science. Since ACOG will not allow me a membership to the Medically Underserved Committee, let me offer this advice based on my 35 years of clinical and professional experience:
- Stop allowing ob-gyn residents to “cut and paste†history and physicals and feign them as their own. This practice represents cheating and does not enhance their clinical acumen. How are residents supposed to learn if they use someone else’s data?
- Initiate mandatory competency exams regarding the diagnosis and management of preeclampsia. Some residents do NOT know how to manage preeclampsia effectively, and I have reviewed those dismal malpractice cases to prove it: The case of the late Dr. Chaniece Wallace is a prime example. The state of Indiana could use some much-needed help.
- Adopt the California Maternal Quality Care Collaborative’s clinical guidelines that have proven they can reduce maternal mortality. The present ACOG clinical guidelines for the management of preeclampsia are as clear as mud, especially as it relates to patients who demonstrate preeclampsia symptoms before 39-weeks. My late residency director, Dr. Sterling Williams, former V.P. of Education at ACOG, is greatly missed. We did not have confusing clinical guidelines when he was alive.
I wish you a successful year as the new ACOG president and hope you will consider some of my recommendations.
Respectfully,
Linda Burke (formerly Burke-Galloway), MD, MS, FACOG